We are delighted to share Dr. Lawrence Recht‘s insights on Intracranial Pressure (ICP) monitoring and related issues.
Dr. Recht serves as a Professor of Neurology at Stanford University, where he has been contributing to the field for over 20 years. He holds the prestigious position of Chief of Neuro-Oncology at Stanford, and chairs the Stanford Cancer Center Scientific Review Committee.
In this engaging Q&A interview, he shares valuable insights into his work, the importance of spinal fluid, ICP monitoring and his thoughts on emerging techniques and their applications in the diagnosis and treatment of various neurological disorders.
Not only will you find the video of the interview, but we have also provided a comprehensive transcript.
Transcript
Question: Could you please introduce yourself?
Dr. Recht: I’m a neuro-oncologist who works in the clinic and in the laboratory, I’ve been at Stanford for 20 years. I run the adult neuro-oncology division.
Question: How is Intracranial Pressure monitoring important?
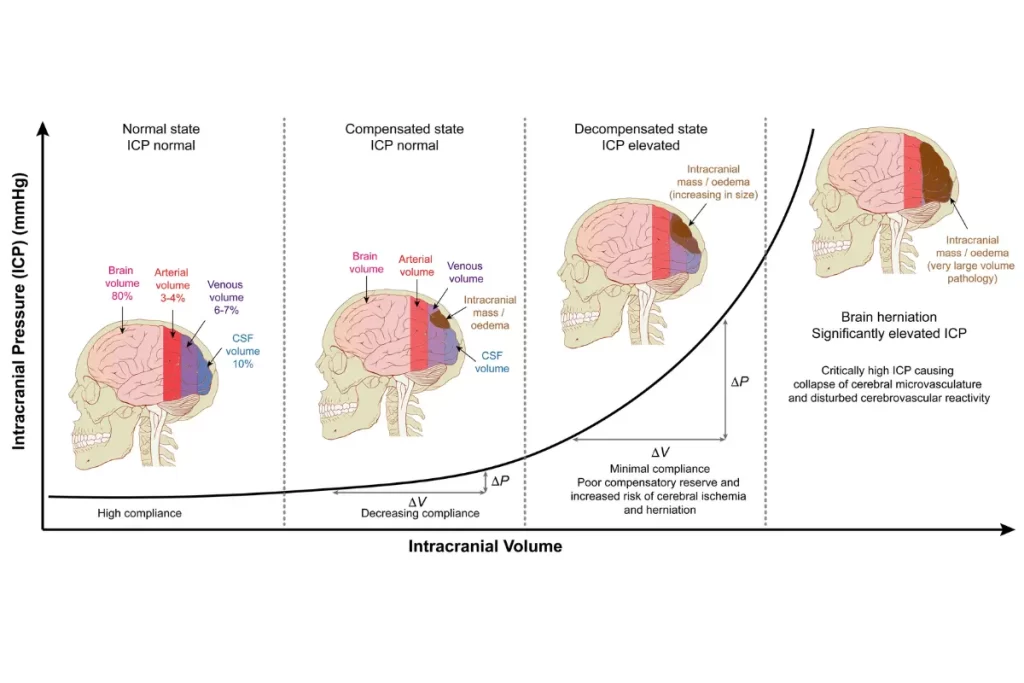
Dr. Recht: Yes. You know, for someone not really involved in neurology, I mean, the spinal fluid bathes the brain. And so it takes up both it’s important in brain circulation and delivering stuff to the brain nutrients and taking waste products away. And it also is an important cushion for the brain. So that the spinal fluid by bathing the brain, the brain lives in a very closed box in which it really does and the brain itself does not like to be shaken. So the CSF provides a lot of the cushion for the brain to work effectively.
Question: What are the common conditions that require ICP monitoring?
Dr. Recht: So because the brain is in a very tight box, when things grow in the brain, it will, that is the most obvious way that the spinal fluid will be impaired both in it because it it requires enough room for the circulation. And when things start growing within the brain, the incirculation is impaired. And this creates a need for the spinal fluid to compensate and that raises the pressure.
So the CSF pressure is a window into understanding what the brain’s capacity, how much, let’s say the skull’s capacity to handle the brain. And both sides of the equation is very finely equilibrated. So that both when it gets too much mass and too little mass and the too little mass is. So when something is pulling from below, you get problems high and low pressure respectively. And those are problems that are quite common, commonly encountered clinically, by people in a neurological specialities.
Question: In which diseases is ICP an indicator?
Dr. Recht: So, masses will raise intracranial pressure. Masses are tumors, masses can be infections. These masses could be located within the substance of the brain. They could be also located on the surface. All of these can change spinal fluid pressure and cause symptoms that could be quite dramatic and potentially lethal when they are at their most extreme. But besides the masses, the spinal fluid circulation itself changes over the course of life and in response to many things and that in itself can be a cause of headaches without any mass effect at all.
And this is probably the most common situation in which pressure monitoring could be very helpful, especially in a chronic stage because these patients are always symptomatic. And it would be nice for the practitioner to be able to understand under what conditions pressure is being affected. And therefore, when you plot out a way to relieve symptoms, it could be very, very valuable.
Question: How is ICP monitoring done currently?
Dr. Recht: Right now, in order to monitor spinal fluid pressure, accurately, you can do it inaccurately in some non-invasive ways. But in order to accurately do it, you have to put some kind of a a tube into the spinal fluid compartment. And this could be done either in the back or through the skull. And then, you can actually link that to a way of measuring pressure.
So in the spine, it’s commonly done in a procedure called a spinal tap, which many people have undergone. This is a temporary measure which has minimal side effects, but patients find it not particularly appealing. And it can also be measured by making a little hole in the skull so that you can sink a catheter into the ventricles, which are these big areas where the CSF pools and you can measure and then you would leave it in. And this is called an intraventricular monitor that also will give you a way of measuring spinal flood pressure.
Question: What kind of treatment decisions can be made by monitoring ICP?
Dr. Recht: So, with tumors which can be very complicated and have a lot of other kinds of problems. The use of spinal fluid monitoring could have major implications, treatment implications in terms of acute quick lowering of spinal fluid pressure. So spinal fluid pressure is not constant, it really fluctuates a lot during the day. So that being able to correlate and know that the headache is due to increased pressure would allow you to better use medications like steroids. You don’t want patients on more steroids than necessary. So you wouldn’t want to treat, every patient patients should not be on steroids all the time, but it could be times where an acute steroid pulse would be able to help them.
You know, in patients with cronic headaches or that are either due to low and high pressure. That also would give the doctor time to both change medications to keep it either to lower the amount of spinal flood production, you can do that with medication. Or other factors that can help, a number of other medicines that could be used in the situation depending on the spinal flood pressure.
Question: Is long-term minimally invasive monitoring of spinal fluid pressure effective?
Dr. Recht: Patients with brain tumor get into problems during their course. And sometimes it’s very difficult to know whether the problem is due to increased spinal fluid pressure or seizures, or the mass effect itself, having a monitor of the spinal fluid pressure, chronically will allow you to actually sort that out quite well. And it also could make big impacts in what you do for treatment.
So yes, having something that could be non-invasively used to measure spinal fluid pressure could be very valuable. The thing is with this is that this has not really been able to be done very well yet. So we don’t have background on this. So this is the other thing that there is much here that hasn’t been that can’t be accomplished even in animals where you can have free running measure of the spinal fluid. So I would anticipate that it would be very as we use it more, we’ll find better its application.
Question: Can accurate monitoring of ICP lead to new studies?
Dr. Recht: You know, there is a lot that people would like to really understand better about the spinal fluid pressure. It’s more than just blood pressure. It doesn’t correlate, you can’t use those kind of distant measures to really, those are not translatable. This is its own separate circulation.
And as we learn more and understand better the fluctuations and under which they occur, I have no doubt that we’ll be able to refine our approaches to many diseases. And I’m sure that some of these, you know, we’re not even, we haven’t even anticipated yet.
Question: Can you talk about the relation between Hydrocephalus and ICP?
Dr. Recht: Yes. well, hydrocephalus is an interesting application. So the treating hydrocephalus is usually done with shunting. But when you should put the shunt in, it’s not really clear. This is especially true in the older population.
And you know, the older population is one of the fastest growing segments of our population. They can develop pressure problems in the nervous system. It could be very hard to diagnose. And more importantly, it’s very hard to know which patients should be shunted or not. And therefore this could be an invaluable way of actually making the decision about which patients would benefit from a shunt.
Up until now, even at this time, the way you measure it is with the spinal tap. It’s convenient for both the patients and the clinics for making time and measuring that. So that having this kind of monitor would obviate that. I think it would change the management of hydrocephalus moving forward.
Question: Is Intracranial Pressure a window to the brain?
Dr. Recht: A lot of this is speculative again because nobody’s really been able to measure chronic pressure for a long time. But you know, much of the brain’s activity manifests itself through the spinal, you know, the spinal fluid circulation and showing disturbances and many patients in clinic have transient disturbances which is very hard to characterize.
So being able to study pressure over the long term would have the same benefit as in the hypertensive patient where they’re measuring blood pressure on a 24 hour monitor, because the fluctuations could be very significant. And if we’re just measuring it at one point in time and in the spinal tap, we’re never going to see these fluctuations which could be very helpful.
Question: How is continuous ICP monitoring beneficial for patients?
Dr. Recht: Well, if you had a way to measure pressure, there will be opportunities for affecting treatment. So if you knew that the pressure was elevated at specific times of the day, you could perhaps modulate, you know, and that correlated with symptoms, you have a very nice baseline from which to measure, you know, to treat and you could be very specific about your treatment.
This would be applicable to areas, you know, either with or without a mass associated with the changes in pressure and frankly, the changes in pressure as long as they’re consistent, gives you ideas of really will open up ideas for creative care, which is really important in medicine because they will generate ideas, you know, that have not been possible. We always assume that pressure is stable. We don’t think about changes in blood in brain pressure because we don’t really have the tools to see what happens during the day or how this fluctuates during the day.
So yes, it could be a great therapeutic opportunity if you could actually measure the pressure and have it in a a readout device. So a doctor could get it and they could read it like any like a EKG or EEG or even a blood pressure monitor.
Yes. Just to use an analogy, I mean, blood pressure monitoring has changed, you know, that’s probably the single most important public health advance in the 20th century and now for, you know, increasing lifespan.
So, whether that could be applicable with a similar approach to spinal fluid honestly not sure, but you could see that there might be great applications that just changing the pressure itself might really have secondary effects on brain function.